Liver Cancer: An Overview
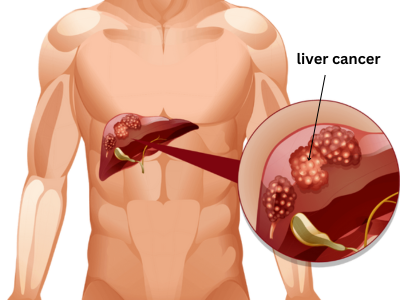
Liver cancer, also known as hepatocellular carcinoma (HCC) in most cases, begins in the cells of the liver, the body’s largest internal organ. The liver performs essential functions such as filtering toxins from the blood, producing bile for digestion, storing nutrients, and regulating blood sugar and cholesterol. Primary liver cancer originates in the liver itself, while secondary (metastatic) cancer spreads to the liver from other parts of the body.
The most common type is hepatocellular carcinoma, which starts in the main liver cells called hepatocytes. It often develops in people with chronic liver conditions. Other rarer forms include intrahepatic cholangiocarcinoma (starting in bile ducts) and angiosarcoma.
Risk Factors, Symptoms, and Early Detection Challenges
Chronic liver damage is the primary driver of liver cancer. Key risk factors include long-term infections with hepatitis B or hepatitis C viruses, which cause ongoing inflammation and scarring (cirrhosis). Other factors involve excessive alcohol consumption leading to alcoholic liver disease, non-alcoholic fatty liver disease often linked to obesity and diabetes, exposure to certain toxins like aflatoxins from moldy foods, and inherited conditions affecting iron or copper metabolism.
In India, chronic hepatitis B and C remain significant contributors, alongside rising cases related to lifestyle factors like fatty liver disease.
Symptoms often appear only in later stages, making early detection difficult. Common signs include unexplained weight loss, loss of appetite, persistent fatigue, upper abdominal pain or swelling, nausea, jaundice (yellowing of the skin and eyes), and fluid buildup in the abdomen.
Diagnosis typically involves blood tests (such as for tumor markers like alpha-fetoprotein), imaging studies (ultrasound, CT, or MRI), and sometimes a biopsy. High-risk individuals benefit from regular screening with ultrasound and blood tests.
Treatment Approaches and Management
Treatment depends on the tumor’s size, location, number, and the patient’s overall liver function and health. For early-stage disease confined to the liver, options include surgical removal of the tumor (partial hepatectomy) or liver transplantation, which replaces the diseased liver with a healthy one.
For cases where surgery is not possible, local therapies such as ablation (using heat, cold, or chemicals to destroy tumors) or embolization (blocking blood supply to the tumor) are used. Systemic treatments like targeted therapies (drugs that attack specific cancer cell features) and immunotherapy (helping the immune system fight cancer) are options for advanced disease. Radiation therapy and chemotherapy may also be considered in certain situations.
Multidisciplinary care involving hepatologists, oncologists, surgeons, and interventional radiologists provides the best outcomes. Prevention focuses on vaccination against hepatitis B, treating hepatitis C, limiting alcohol, maintaining a healthy weight, managing diabetes, and avoiding toxin exposure.
Early awareness and management of liver conditions can significantly impact outcomes. If you have risk factors or notice concerning symptoms, consult a healthcare specialist promptly for evaluation and guidance.
