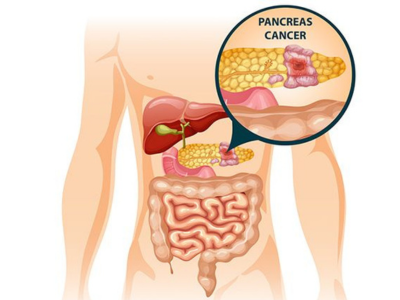
Pancreatic Cancer: An Overview
Pancreatic cancer occurs when abnormal cells begin to grow uncontrollably within the pancreas. The most common form originates in the ducts that carry digestive enzymes, while less common types arise from hormone-producing cells. The disease is known for its aggressive nature and ability to spread to nearby organs if not detected early. Prompt evaluation by an experienced cancer specialist plays a crucial role in accurate diagnosis and timely treatment planning.
Common Symptoms and Early Warning Signs
In the initial stages, pancreatic cancer may not cause noticeable symptoms. As the tumor grows, patients may experience:
Persistent upper abdominal pain that may extend to the back
Unintentional weight loss and reduced appetite
Yellowing of the skin or eyes (jaundice)
Digestive problems such as bloating or fatty stools
Extreme tiredness or weakness
New-onset diabetes or worsening blood sugar control
Because these symptoms can overlap with other conditions, early medical consultation is essential when symptoms persist or worsen.
Risk Factors and Prevention
Several factors can increase the risk of developing pancreatic cancer, including advancing age, smoking, obesity, long-standing diabetes, and chronic inflammation of the pancreas. A family history of pancreatic or related cancers may also raise risk. While not all cases can be prevented, maintaining a healthy lifestyle, quitting smoking, and managing metabolic conditions may help reduce overall risk.
Diagnosis and Treatment Approach
Diagnosis involves advanced imaging techniques such as CT scans or MRI, blood investigations, and sometimes tissue biopsy. Once confirmed, treatment depends on the cancer stage, location, and the patient’s overall health.
Treatment options may include:
Surgical removal of the tumor when detected early
Chemotherapy to control or shrink cancer cells
Radiation therapy in selected cases
Supportive and palliative care to manage symptoms and improve quality of life
A multidisciplinary cancer care team ensures a personalized treatment plan focused on both survival and well-being.
